Nasal Polyps
Current Studies: Call 515-225-6050 to see if the following study might be right for you or fill out a personal contact form.
Support Resources:
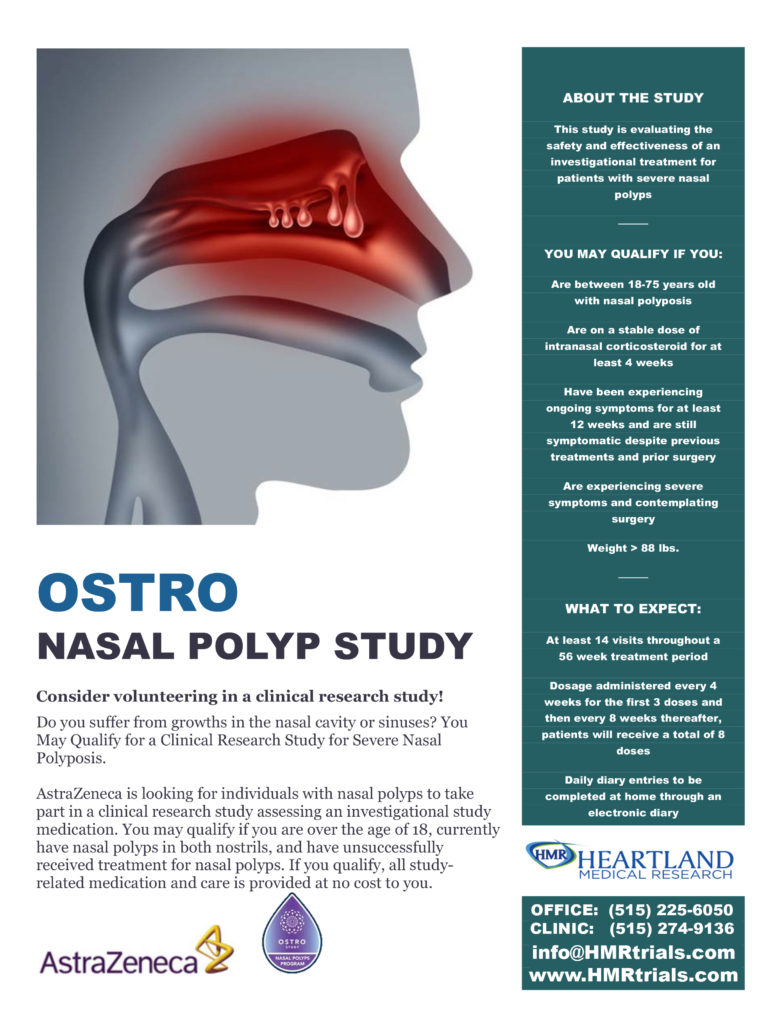
What Are Nasal Polyps?
Nasal polyps are soft, painless, noncancerous growths on the lining of your nasal passages or sinuses. They hang down like teardrops or grapes. They result from chronic inflammation due to asthma, recurring infection, allergies, drug sensitivity or certain immune disorders.
Small nasal polyps may not cause symptoms. Larger growths or groups of nasal polyps can block your nasal passages or lead to breathing problems, a lost sense of smell and frequent infections.
Nasal polyps can affect anyone, but they’re more common in adults. Medications can often shrink or eliminate nasal polyps, but surgery is sometimes needed to remove them. Even after successful treatment, nasal polyps often return.
What Are The Symptoms?
Nasal polyps are associated with inflammation of the lining of your nasal passages and sinuses that lasts more than 12 weeks (chronic rhinosinusitis, also known as chronic sinusitis). However, it’s possible — and even somewhat more likely — to have chronic sinusitis without nasal polyps.
Nasal polyps themselves are soft and lack sensation, so if they’re small you may not be aware you have them. Multiple growths or a large polyp may block your nasal passages and sinuses.
Common signs and symptoms of chronic sinusitis with nasal polyps include:
- A runny nose
- Persistent stuffiness
- Postnasal drip
- Decreased or absent sense of smell
- Loss of sense of taste
- Facial pain or headache
- Pain in your upper teeth
- A sense of pressure over your forehead and face
- Snoring
Causes
Scientists don’t yet fully understand what causes nasal polyps. It’s not clear why some people develop chronic inflammation or why ongoing inflammation triggers polyp formation in some people and not in others. The inflammation occurs in the fluid-producing lining (mucous membrane) of your nose and sinuses. There’s some evidence that people who develop polyps have a different immune system response and different chemical markers in their mucous membranes than do those who don’t develop polyps.
Nasal polyps can form at any age, but they’re most common in young and middle-aged adults. Nasal polyps may form anywhere in your sinuses or nasal passages, but they appear most often in an area where sinuses near your eyes, nose and cheekbones all drain through winding passages into your nose (ostiomeatal complex).
Risk factors
Any condition that triggers chronic inflammation in your nasal passages or sinuses, such as infections or allergies, may increase your risk of developing nasal polyps. Conditions often associated with nasal polyps include:
- Asthma, a disease that causes overall airway inflammation and constriction
- Aspirin sensitivity may cause some people to be more likely to develop nasal polyps
- Allergic fungal sinusitis, an allergy to airborne fungi
- Cystic fibrosis, a genetic disorder that results in the production and secretion of abnormally thick, sticky fluids, including thick mucus from nasal and sinus membranes
- Churg-Strauss syndrome, a rare disease that causes the inflammation of blood vessels
Your family history also may play a role. There’s some evidence that certain genetic variations associated with immune system function make you more likely to develop nasal polyps.
Complications
Nasal polyps can cause complications because they block normal airflow and fluid drainage, and also because of the chronic inflammation underlying their development. Potential complications include:
- Obstructive sleep apnea. In this potentially serious condition, you stop and start breathing frequently during sleep.
- Asthma flare-ups. Chronic rhinosinusitis can aggravate asthma.
- Sinus infections. Nasal polyps can make you more susceptible to sinus infections that recur often or become chronic.
Prevention
You may help reduce your chances of developing nasal polyps or having nasal polyps recur after treatment with the following strategies:
- Manage allergies and asthma. Follow your doctor’s treatment recommendations for managing asthma and allergies. If your symptoms aren’t well-controlled, talk to your doctor about changing your treatment plan.
- Avoid nasal irritants. As much as possible, avoid breathing airborne substances that are likely to contribute to inflammation or irritation of your nose and sinuses, such as allergens, tobacco smoke, chemical fumes, and dust and fine debris.
- Practice good hygiene. Wash your hands regularly and thoroughly. This is one of the best ways to protect against bacterial and viral infections that can cause inflammation of the nasal passages and sinuses.
- Humidify your home. Use a humidifier if the air in your home tends to be dry. This may help moisten your breathing passages, improve the flow of mucus from your sinuses, and help prevent blockage and inflammation.
- Use a nasal rinse or nasal lavage. Use a saltwater (saline) spray or nasal lavage to rinse your nasal passages. This may improve mucus flow and remove allergens and other irritants.You can purchase over-the-counter saline sprays or nasal lavage kits with devices, such as a neti pot, to administer a rinse.If you make your own rinse, use water that’s distilled, sterile, previously boiled and cooled, or filtered using a filter with an absolute pore size of 1 micron or smaller to make up the irrigation solution. Also be sure to rinse the irrigation device after each use with similarly distilled, sterile, previously boiled and cooled, or filtered water and leave open to air-dry.
Source: Mayo Foundation for Medical Education and Research (MFMER). 1998-2018. Nasal Polyps. https://www.mayoclinic.org/diseases-conditions/nasal-polyps/symptoms-causes/syc-20351888